What is an aneurysm and what causes it?
The aorta is the main artery that originates from the heart and supplies blood from to the rest of the body. There are major branches from the aorta that supply blood to the brain, limbs and vital organs.
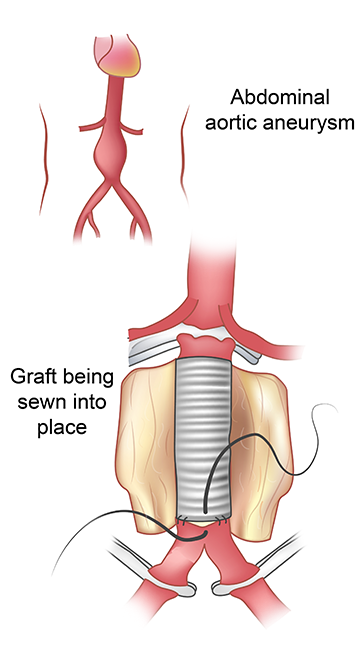
An aortic aneurysm is an expansion of the wall of the aorta beyond its normal size. Like a balloon, once the tension in the wall reaches a critical level the aorta can rupture resulting in a critical situation and shock that can lead to death. It is therefore very important to treat an aneurysm before this dangerous situation occurs. An aneurysm may occur in any part of the aorta but it is by far most common in the abdominal portion below the branches to the vital organs. The cause of an aneurysm is not completely understood. However, the risk factors include, family history, smoking, uncontrolled hypertension and uncontrolled elevated cholesterol. The underlying problem is a weakness in the wall of the artery which we do know has a hereditary component and is also worsened by smoking and uncontrolled high blood pressure. It is more common in men, but women are also frequently affected.
What are the symptoms of an aortic aneurysm?
An aneurysm may cause chest pain, abdominal pain, or back pain, depending on its location. However many aneurysms produce no symptoms and are discovered incidentally during a physical examination, screening exam, or on diagnostic testing performed for other reasons.
What are the diagnostic tests commonly used to identify aneurysms?
Ultrasound is a very common, non invasive, and excellent screening test for an abdominal aortic aneurysm. Medicare covers a screening exam for men above age 65 who have smoked more than 100 cigarettes in their lifetime. In addition, anyone who has a family history of aortic aneurysm should consider requesting a screening Aortic Ultrasound from their physician. If an aneurysm is found on ultrasound a CT scan may then be requested. The CT scan will provide more information about the size and anatomy of the aneurysm and is particularly important if treatment is necessary. The patient should fast for the ultrasound exam so that the aneurysm can be imaged better. A simple blood test may be required prior to the CT scan if IV contrast is administered.
How is an abdominal aortic aneurysm treated?
Watchful waiting
The size of the aneurysm is very important to determine the treatment. If the aneurysm is Asymptomatic, located in the abdomen and is less than 5 cm or if located in the chest and less than 6 cm, close follow up may be indicated because below these sizes the risk of rupture is lower than the risks for operative repair. Your surgeon will likely choose to follow an aneurysm of this size every 6 to 12 months with either ultrasound or CT scan. Your surgeon will also recommend control of high blood pressure, smoking cessation and avoidance of constipation or severe straining or weight lifting. These are all risk factors associated with aneurysm expansion. In addition, regular exercise has been shown to be beneficial to reduce aneurysm expansion and a walking program 30 minutes daily at least 5 times a week is strongly encouraged. There are special cases where an aneurysm smaller than this may need repair. These cases involve either a rapid growth of the aneurysm, an aneurysm that is causing pain, or if the aneurysm is a focal outpouching of the wall (known as saccular aneurysm) rather than a general dilation of the whole segment of the artery (known as fusiform aneurysm). These focal outpouchings called saccular aneurysms are more dangerous and may require repair at smaller sizes.
If an aneurysm requires repair, there are two options. Most patients are now treated with endovascular stent grafts. These are large covered stents which are inserted through the arteries in the groin area and internally bypass and exclude the aneurysm from the circulation. The advantage to this approach is a rapid recovery and short hospital stay. Patients are able to resume eating the day of the procedure and usually are discharged the following day and able to resume most normal activities shortly after discharge. Some patients, however, do not have enough normal aorta to seal the aneurysm with the stents and require an open surgical repair. This operation definitely repairs the aneurysm by replacing it with a graft that is sewn onto the aorta. However, because a major body cavity is entered, the surgery requires approximately 4 to 7 days in the hospital and a longer overall recuperation period at home.
How are patients followed after surgery?
Patients with an aortic graft will require lifelong follow up with their surgeon. It is also important to take prophylactic antibiotics prior to any invasive procedures, including dental procedures to prevent infection of the graft. The follow up for patients with endovascular repair is often more frequent because the stent needs to be checked periodically to ensure a continued seal of the aneurysm. Normal follow up is at 2 weeks, 3 months post procedure, 6 months post procedure, and then yearly. These follow up visits will usually be accompanied by a CT scan or ultrasound or both to evaluate the stent. The follow up after open surgery usually doesn't require further imaging tests.
THORACIC AORTIC ANEURYSM
Thoracic aortic aneurysms are usually asymptomatic, making them difficult to detect and grow slowly. As they grow, they can compress nearby structures and cause Chest or Back pain, Chronic Cough, hoarseness in the voice, and Shortness of breath
As Thoracic aortic aneurysm grow, they can rupture or cause dissection. In this setting the symptoms can include: Sharp sudden upper back and/ or chest pain, Difficulty breathing, Low blood pressure, Shortness of breath and Trouble swallowing.
Depending on the location of the thoracic aortic aneurysm, they my be treated with stent grafts through groin access ( in the case of Descending thoracic aneurysm or dissection), or may need open repair ( in the case of Ascending and Arch aneurysm and dissection).
CT Angiogram can define the anatomy and your surgeon can recommend appropriate treatment.