What is Aortoiliac Occlusive Disease?
The aorta is the main blood vessel that arises from the heart and supplies the vital organs and extremities with oxygenated blood. In the pelvic area the area branches into the iliac arteries which are the main supply of blood to the legs. Aorto iliac occlusive disease is a form of peripheral arterial disease or PAD that affects aorta and iliac arteries. The disease is due to plaque buildup within the walls of the arteries that obstructs the flow of blood to the pelvis and to the extremities.
What causes Aortoiliac Occlusive Disease?
This plaque buildup in the aorta and iliac arteries may be caused by several risk factors for blood vessel disease. Family history is an important component, as is smoking cigarettes, high cholesterol, high blood pressure, and diabetes.
What are the symptoms of Aortoiliac Occlusive Disease?
Patients may experience pain in the muscles of the legs when walking because the muscles are not receiving adequate oxygen. These symptoms may be worse when walking uphill or rapidly and are usually relieved with rest. Patients may also experience pain with walking in the hips or buttocks because these muscles are supplied by the iliac arteries. Males may also have erectile dysfunction. Patients with severe disease may have pain continually in the legs due to lack of circulation. This may be worse at night because the legs are elevated and gravity doesn't help the blood reach the lower legs and feet. This pain may be relieved by placing the legs in a dependant position. Patients with severe disease may also have non healing wounds or gangrene.
How is Aortoiliac Occlusive Disease Diagnosed?
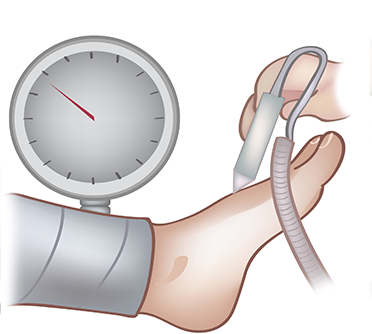
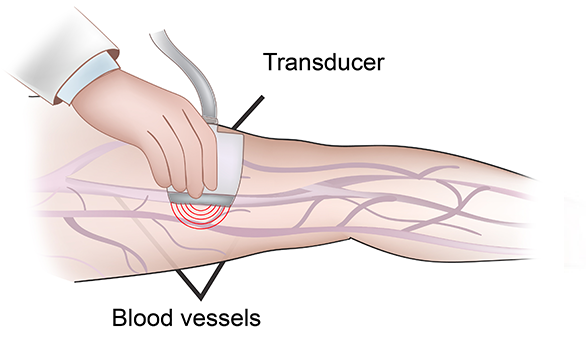
Your physician will first order an arterial ultrasound exam. This non-invasive exam allows us to determine where the blockage is. We will also measure pressures at the ankle and at the toes to help determine how severe the overall disease is.These pressures may be done at rest and then after foot flexion exercise which can be helpful to determine if the symptoms are from vascular disease. If treatment is needed, your physician will likely need to perform a test with contrast to better image the arteries. This may be done with either a CT scan angiogram or MRI angiogram or with an angiogram where dye is directly injected through a small puncture site in the leg artery in the groin area depending on what type of treatment is anticipated.
What are the treatments for Aortoiliac Occlusive Disease?

First and vitally important is that all risk factors for vascular disease should be treated. This means smoking must be stopped, cholesterol, diabetes and high blood pressure all well controlled. If these are not controlled, any treatment that is done may not be durable.
For patients who have pain with walking but no rest pain or gangrene, a trial of exercise therapy may be advised. Patients will be asked to walk at least 5 times a week for 30 minutes. Walking should be done to the point of muscle pain and then continued for a short period. Patients should then rest until the pain resolves and then begin walking again. This will encourage new blood vessel formation and often will greatly improve the walking distance so that procedures are not required. The exercise therapy may be accompanied with a medication called pletal which can dilate blood vessels and improve walking distance.
For patients who fail exercise therapy and are disabled by their leg pain a procedure may be required to improve blood flow. Similarly if a patient has severe disease with rest pain or non- healing wounds a procedure will likely be needed.
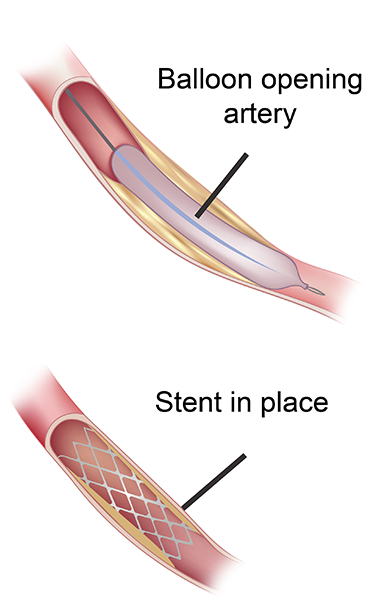
If the blockages are relatively short, they may be treated with an angioplasty or stent placement. This is done through the insertion of a small flexible tube in the femoral artery in the groin. Through this insertion site, we can place a balloon to dilate the artery and if needed a stent to hold it open improving the blood flow. The recovery from these procedures is rapid and they may even be done as an outpatient in our office depending on the circumstances. If the blockages are longer, it may not be possible to treat with stenting. In these circumstances a bypass surgery may be required in the hospital. This surgery usually requires several days in the hospital and a longer recuperation time.
How Will I Follow Up After the Procedure?
Unfortunately vascular disease cannot be "cured" by a procedure. Although blockages may be stented or bypassed they can recur and even become worse. It is therefore very important to follow up with your surgeon regularly. Depending on your procedure, ultrasounds may be requested periodically to evaluate the revascularized artery to ensure that it remains durable. Continued optimization of all risk factors is a critical component to success and cannot be emphasized enough.