What is a DVT?
The veins return the blood from the extremities and organs to the right side of the heart so that the blood can be pumped into the lungs to receive oxygen. Any of these veins may have a blood clot form within them. If the clot forms within one of the deep veins of the extremities or abdominal cavity the clot is called a deep vein thrombosis or DVT.
What causes DVT?
In the 1800s a famous physician named Rudolf Virchow identified 3 factors called Virchow's triad which lead to clot formation. These conditions may act singly or in combination to form a clot. One of these conditions is stasis which means a condition that impairs or slows the flow of blood. When a patient is immobile for long periods, the flow of the blood in the leg veins is reduced because the muscles are not contracting to push blood up out of the legs. This is why DVT may sometimes occur after surgeries when a patient is in bed or casted or when someone has been sitting for a long time such as on an extended flight or car trip. Another condition is trauma which may damage the wall of the vein. The body's response to this injury is clot formation. An example of this is the clot that sometimes is seen after certain types of IV lines are placed. The final condition is an abnormal tendency toward clotting of the blood itself, called a hypercoagulable state. This may be inherited genetically or may occur with certain types of illnesses such as cancer or autoimmune disease.
What are the symptoms of DVT?
DVT may produce swelling or pain in the affected extremity. Sometimes there may be very subtle or even no symptoms in the extremity. If the DVT moves from the leg and goes through the heart into the lungs it can be very serious and cause chest pain, shortness of breath, bloody sputum,, rapid heart rate, and dizziness or even complete loss of consciousness.
How is DVT diagnosed?
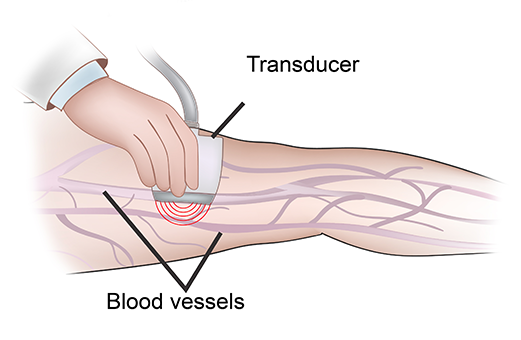
The venous ultrasound exam is the main test used because it can visualize the blood clot within the veins of the extremities and is very sensitive for the condition. If the clot is suspected to be within the abdominal cavity or lungs then a CT scan with IV contrast administration will be needed. There is a blood test called d-dimer which can raise your doctor's suspicion of a DVT but it can't definitively confirm it.
How is DVT treated?
Treatment depends on how extensive the DVT is, what other health conditions the patient has, and what caused the DVT.
For the patient who has a clear cause which led to or provoked the DVT such as a long flight or surgery, treatment will usually begin immediately with medicines to thin the blood called anticoagulants. These medications, described in more detail below, prevent the DVT from worsening and allow the body's own clot dissolving system to gradually break the clot down over several weeks to months. This treatment will usually need to be done for 3 months with a repeat ultrasound toward the end of treatment to assess how well the clot has dissolved.
For the patient without clear cause of the DVT and who therefore have "unprovoked" DVT, the same treatment will be required but because there is a higher risk of recurrence since we don't know why the clot formed the treatment needs to be continued longer. At least 6 months is usually required and sometimes the treatment is continued indefinitely. Patients in this category will need blood testing to check for an underlying clotting disorder. It is also very important to make sure the patient is in good health and is up to date on all age appropriate health screening such as mammograms, colonoscopy, pelvic, and prostate exams. A referral to a hematology doctor is often done to pursue further evaluation.
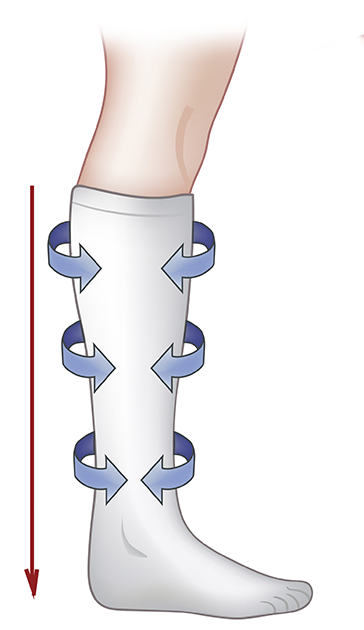
Most patients with DVT will have swelling at least initially and some compression stockings are very helpful to reduce the swelling
What happens if a patient cannot take the blood thinning medications?
Some patients may have a contraindication to taking the blood thinning medications such as a recent surgery or active bleeding. For these patients there is a danger that the DVT within the extremity could travel to the lung resulting in life threatening breathing problems. In a patient with DVT of the lower extremities who cannot take the blood thinning agent, an inferior vena caval filter (IVC filter) is recommended. IVC filters do not treat the DVT in the lower extremities but they can act as a screen to prevent the clot from reaching the lungs. Many patients are nervous about IVC filters because they have seen negative ads about them on television. We do not recommend them for everyone, but when needed they can be lifesaving. There is more information about IVC filters in our procedures section.
What happens if the leg is massively swollen and the blood thinning medications can't reduce it?
Usually DVT is very effectively treated by blood thinning medications. Very rarely, the DVT is so extensive and the leg so swollen that a patient can be at risk for loss of the limb or severe long term disability. In these cases a more active clot dissolving technique may be required. Since this technique uses a very powerful clot dissolving medication and has risks of bleeding it is only used selectively and is not for all patients. This technique, called catheter directed thrombolysis, involves your physician placing a small catheter within a vein of the leg and instilling a clot dissolving medication directly into the DVT. Then the clot can be suctioned out. Sometimes the catheter has to be left in overnite with a slow infusion of the medication.
What are the blood thinning medications available?
Many new medications have become available over the past several years. Prior to this development patient's usually had to be hospitalized and placed on intravenous medications which were overlapped with Coumadin, the only oral medication available in the past. Coumadin requires monitering with blood tests, dietary modifications, and takes several days to become therapeutic. The newer oral agents such as pradaxa, xarelto, or eliquis, work immediately and don't require monitering with blood tests. The main risk with all of these medications is bleeding because they thin the blood. The advantage to Coumadin if bleeding does occur is that we can reverse its effects with a plasma transfusion which is readily available. The disadvantage of course is the monitering required and all of the dietary restrictions in conjunction with the slow time of onset that requires overlap with either an intravenous or injectable medication. Because the newer agents produce a more reliable level of consistent anticoagulation they are now advised for most patients. They have enabled many patients with mild DVT to be treated without hospitalization.
If I am traveling or having surgery should I worry?
Millions of people travel and have surgery and DVT fortunately is very uncommon. A few basic precautions can be very helpful. If you are on a long flight or car trip you can flex your feet and move your legs while sitting every few minutes. You should also try to get up hourly and walk for a few minutes. If you are undergoing surgery and are hospitalized, most patients receive prophylaxis with pumps on the legs and a low dose anticoagulation as a preventative. You should check with your physician to determine what if any prophylaxis for DVT is appropriate for your condition.