What are the options for dialysis access?
Most patients who require dialysis undergo hemodialysis. This type of dialysis requires that the blood run through the dialysis machine to filter out the toxins and then be returned to the patient. Access for this type of dialysis can be placed by your vascular surgeon and may include an AV fistula, AV graft, or dialysis catheter. This type of dialysis is usually performed 3 times a week for 4 hours at the dialysis unit. Some patients may be able to be trained at home if they are highly motivated to perform their own dialysis. The other option for dialysis is peritoneal dialysis. This is done by the patient every day, usually at night when sleeping. The surgeon will place a catheter within the abdominal cavity and the dialysis is done through fluid exchanges.
How is hemodialysis access done?
If the need for dialysis is immediate then a dialysis catheter can be inserted. This is a flexible tube which is usually placed in the jugular vein in the neck and tunneled so that the tubes come out just below the collar bone. This is an outpatient procedure with a very quick recovery. It is not ideal for long term dialysis due to risk of infection and the possibility of narrowing the veins in the chest over time. It must be kept completely dry to reduce infection risks and showering and protecting the catheter can be very challenging.
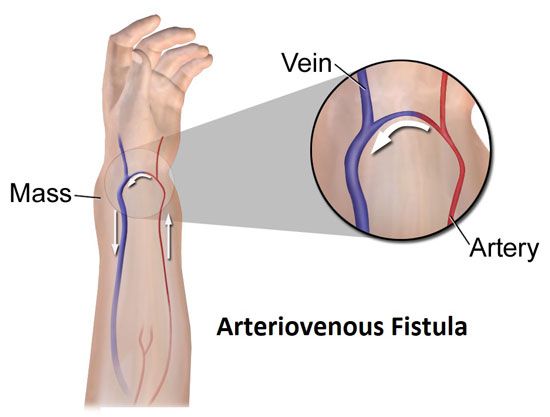
For patients anticipated to require long term dialysis, it is ideal to place an AV fistula. In this procedure, the surgeon will make a small incision at the wrist level or just above the bend in the elbow and connect a vein directly to an artery. Normally the blood will circulate to the hand through the arteries and return gradually through the veins. When an AV fistula is made, a portion of the blood passes directly into the vein and over time the vein will dilate so that eventually dialysis can be done like a blood draw by accessing the fistula with two needles. When the patients are not on dialysis nothing is external and since a fistula is all the patient's own tissue the risk of infection is very low.
Sometimes the patient's veins are too small or too deep for a fistula to be made through a small incision. If the veins are too deep, two stages to the operation will be needed. One to connect the vein and a second stage to make the vein more superficial. If all the veins are simply too small then a synthetic graft may be placed to make a bridge between the artery and veins.
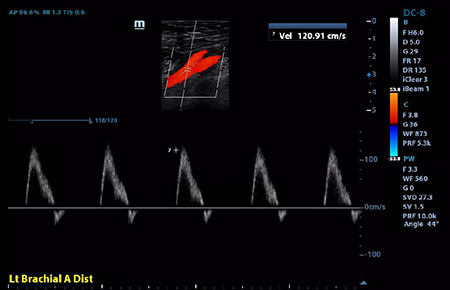
The surgeon determines where to place the fistula by doing ultrasound before surgery to identify where the best veins are located. Once a decision has been made to place a fistula the patient should avoid blood draws or IV in the arm so that the veins do not become damaged. A fistula should be placed as soon as possible after it is determined that long term dialysis is needed because it takes at least 6 weeks to heal after surgery before the fistula can be used. This will minimize the duration that the catheter is needed and minimize the risks of infection.
How often will I see my surgeon after I am on dialysis?
If a patient has good veins a fistula can last for years but it may not last forever. The vein that is connected to the artery may develop scar tissue over time that could cause the fistula to fail. Your surgeon will want to check the fistula periodically to make sure it is functioning normally. If a problem is detected early it can often be fixed in our office with a simple angioplasty which will avoid the need for further surgeries and prolong the life of the fistula.